As people age, their need for healthcare increases—but access to that care often becomes harder. For many older adults, getting timely medical help is not just inconvenient; it’s a daily struggle shaped by mobility issues, cost, distance, technology gaps, and lack of support. Poor access to healthcare in the elderly is a silent crisis—one that worsens outcomes, increases hospitalizations, and diminishes quality of life. The good news is that it can be solved with thoughtful, practical changes at the family, community, and system levels.
Aging brings predictable challenges that compound over time. Mobility limitations make travel to clinics difficult. Chronic conditions require frequent follow-ups. Vision, hearing, or cognitive changes complicate communication with providers. Many elders rely on others for transport and appointment coordination. Add financial constraints and long wait times, and routine care gets delayed—sometimes until an emergency occurs. Rural elders face distance and provider shortages; urban elders face congestion and complex systems. Across settings, digital health tools often exclude seniors who lack smartphones, internet access, or confidence with technology.
When access falters, care becomes reactive instead of preventive. Missed checkups lead to uncontrolled diabetes or hypertension. Untreated pain reduces mobility and independence. Minor infections escalate into hospital admissions. Beyond physical health, the emotional toll—anxiety, helplessness, and isolation—can be profound. Solving access isn’t just about clinics and doctors; it’s about continuity, convenience, and confidence.
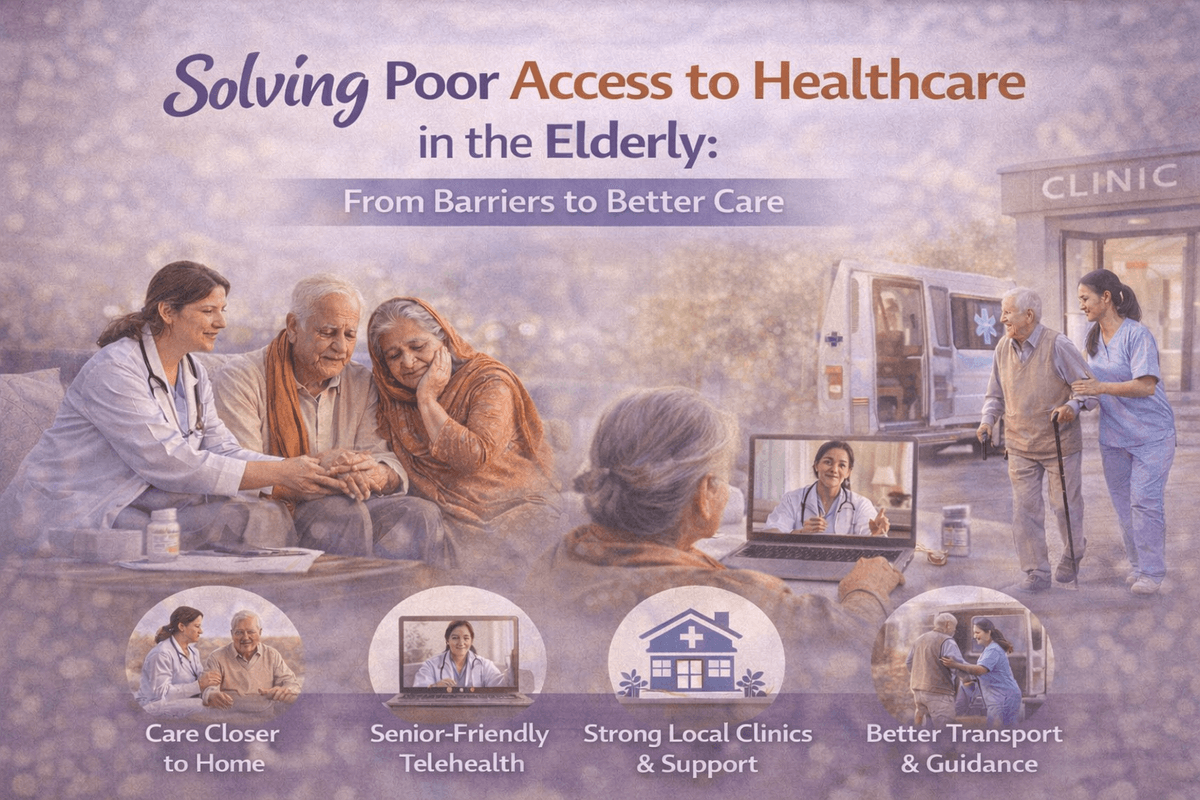
Home-based services—doctor visits, nursing care, physiotherapy, diagnostics, and medication delivery—remove the biggest barrier: travel. Even periodic home visits can prevent deterioration and catch problems early.
Telemedicine works best when designed for elders: simple interfaces, larger text, audio-first options, and caregiver participation. Hybrid models—virtual visits supported by periodic in-person checkups—offer flexibility without sacrificing quality.
Strong local clinics, community health workers, and outreach programs reduce dependence on hospitals. Regular screening camps, vaccination drives, and chronic-disease check-ins bring preventive care within reach.
Caregivers often coordinate appointments, medications, and follow-ups. Training them—briefly and practically—improves adherence and outcomes. Shared care plans and clear communication channels keep everyone aligned.
Dedicated senior transport, appointment batching, and patient navigators who help book visits, explain instructions, and follow up can dramatically reduce drop-offs in care.
Transparent pricing, insurance guidance, and affordable packages for chronic care help seniors seek care earlier. When cost anxiety drops, access improves.
Remote monitoring, fall-prevention strategies, and timely alerts don’t replace doctors—but they bridge gaps between visits and prompt early intervention.
Families play a pivotal role by noticing changes early, encouraging routine checkups, and advocating for accessible options. Communities can create senior-friendly spaces, host health days, and normalize asking for help. Small steps—like a neighbor’s check-in or a local clinic’s reminder call—make a big difference.
True access respects dignity. It avoids making elders “prove” their need, navigate maze-like systems, or depend entirely on others. The goal is simple: care that fits into their lives, not lives contorted around care.
Poor access to healthcare in the elderly isn’t inevitable—it’s solvable. By bringing care closer to home, simplifying technology, empowering caregivers, strengthening community services, and reducing financial and logistical barriers, we can shift from crisis care to continuous, compassionate support. When access improves, outcomes improve—and so does independence, confidence, and quality of life.

Copyright ©2025 ripplehealthcare.in
All Rights Reserved