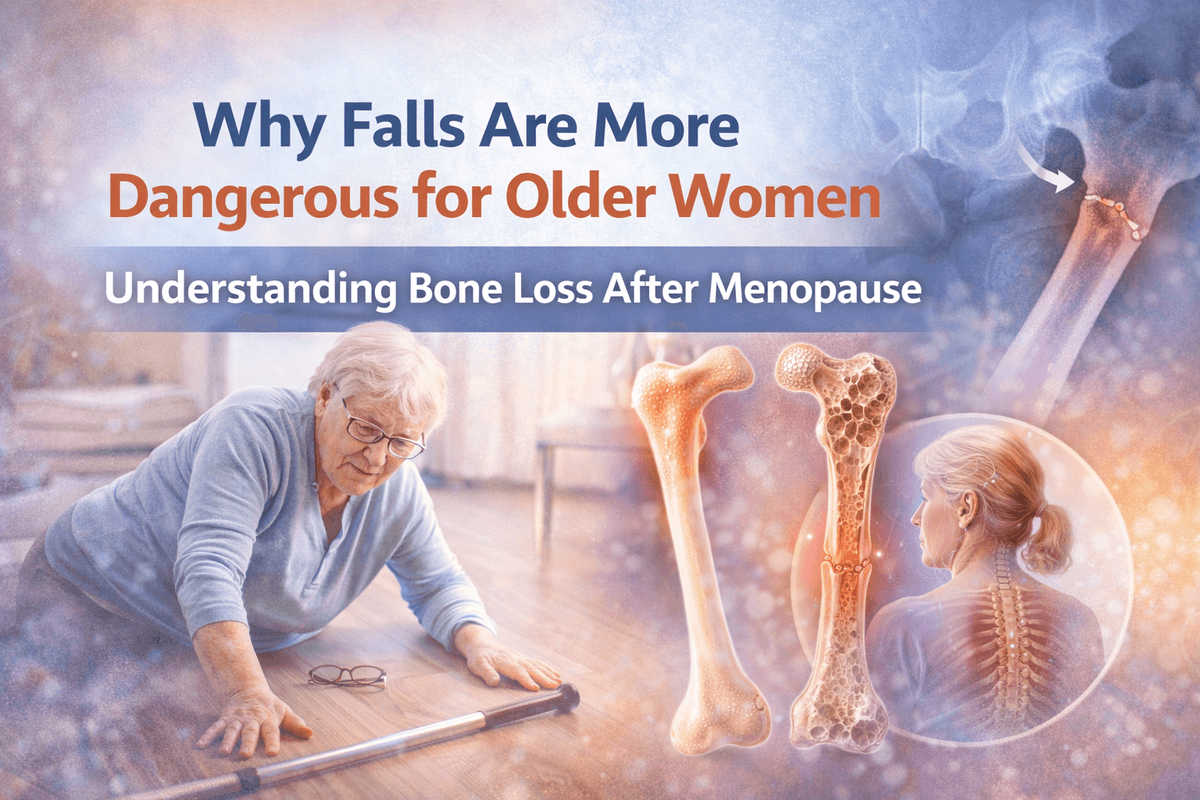
As women age, the risk of falls increases sharply—much more so than in men of the same age. This isn’t coincidence, clumsiness, or “just getting older.” A major driver is bone weakening after menopause, combined with changes in muscle strength, balance, and hormones. Understanding why this happens is the first step toward preventing serious injuries like hip and spine fractures.
Before menopause, estrogen plays a protective role in women’s bones. It helps maintain bone density by balancing bone breakdown and bone formation. After menopause, estrogen levels drop sharply. As a result, bone loss accelerates, especially in the first 5–10 years after menopause. Women can lose up to 20–30% of their bone mass during this period. This condition—osteoporosis—makes bones porous, fragile, and more likely to break even after a minor fall. Men do lose bone with age too, but much more slowly and usually later in life. That difference alone puts older women at a higher risk of fractures when they fall.
Falls happen to both men and women, but women are far more likely to fracture a bone when they fall. Hips, wrists, and the spine are especially vulnerable. A fall that might cause a bruise in a man can lead to a hip fracture in a woman. This is why statistics consistently show:
Higher rates of hip fractures in older women
Longer recovery times after falls
Greater loss of independence following injury
After menopause, women also experience loss of muscle mass and strength, a process called sarcopenia. Weaker muscles mean poorer balance, slower reflexes, and reduced ability to prevent a fall once balance is lost. Additionally, age-related changes such as:
Hip fractures are one of the most serious consequences of falls in older women. Recovery is often slow and incomplete, and many women never regain their previous level of independence. Complications such as infections, blood clots, and reduced mobility are common. This is why fall prevention in women is not just about safety—it is about preserving quality of life, dignity, and independence.
While menopause-related bone loss cannot be completely reversed, its impact can be reduced. Regular bone density screening, adequate calcium and vitamin D intake, weight-bearing exercise, and balance training all play an important role. Addressing vision problems, reviewing medications that cause dizziness, and making homes safer can dramatically lower fall risk. Equally important is awareness. Many women underestimate their fracture risk because they “feel fine” until the first fall happens. Unfortunately, the first fracture is often the warning sign that comes too late.
Older women are not weaker because of age—they are more vulnerable because of biological changes after menopause that affect bones and muscles. Falls in women are more likely to result in serious fractures, especially of the hip and spine. Recognizing this risk early, prioritizing bone health, and actively preventing falls can save mobility, independence, and lives. For women after menopause, fall prevention is not optional—it is essential.

Copyright ©2025 ripplehealthcare.in
All Rights Reserved